Plantar Fasciitis
Pounding Pavements? Protect your Plantar Fascia.
Whether the COVID-19 lockdown caused you to rack up 10K a day, or you have always enjoyed a good walk or run, it goes without saying that heel pain has been a common complaint throughout 2020.
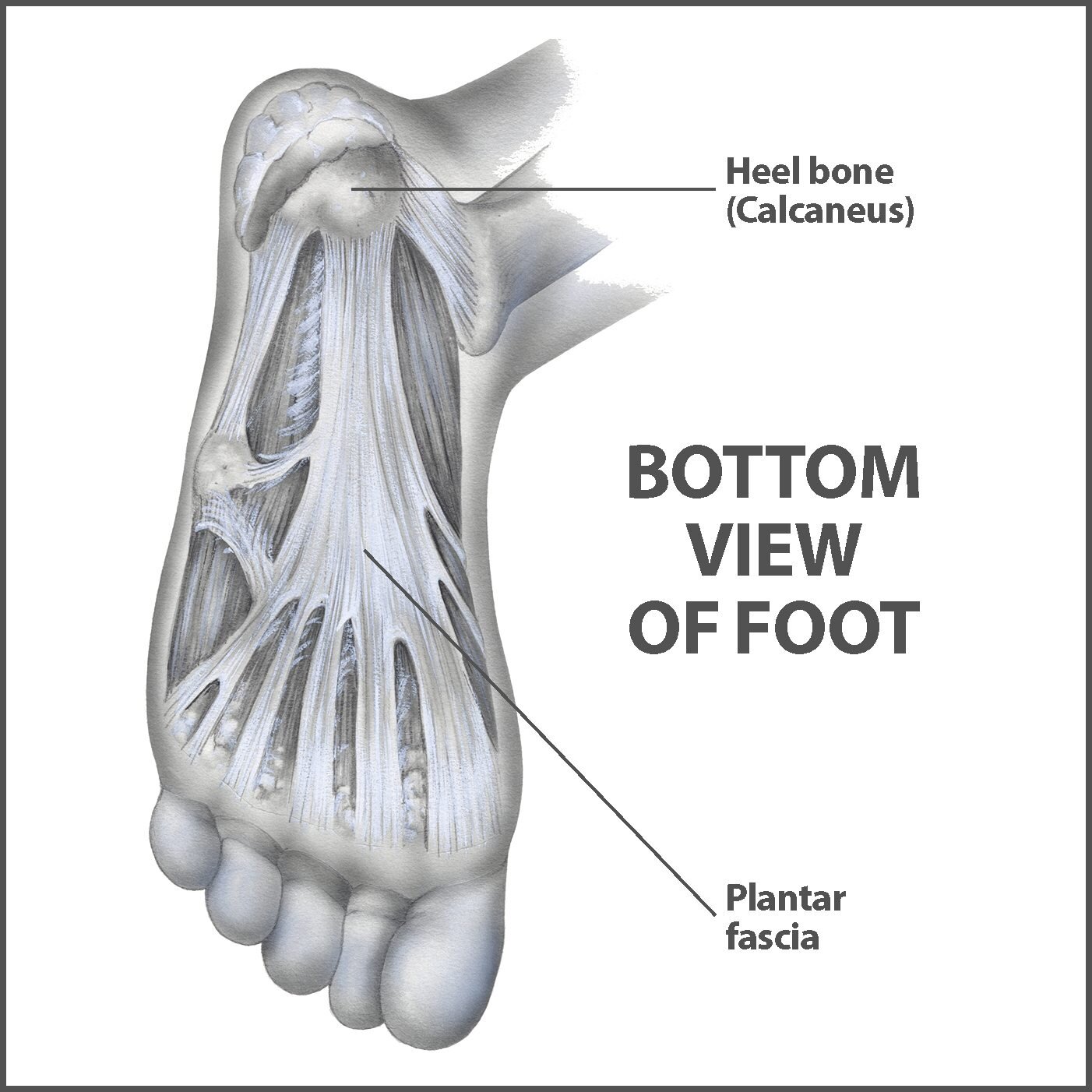
To understand Plantar Fasciitis, we must first know what the Planter Fascia is.
From the diagram, you can see a thick fibrous structure travelling from the base of the heel bone (calcaneus) towards to ball of the foot. This structure is the Plantar Fascia. Fascia is a structure found in every area of the body that helps create stability, tension, and motion within joints. It is formed by a 3-D collagen matrix which means its composition is very similar to that of a tendon (Kumka et al, 2012). This makes the fascia highly adaptable to its environment, and shows a capacity to remodel itself if function changes, such as increasing running or walking distance, or spending long periods of your day on your feet.
What is Plantar Fasciitis?
It was once believed, much like in other overuse injuries (see our Achilles Tendonopathy Blog), that inflammation was the key player in tendon and fascia disorders. More recently, the term plantar fasciosis has been introduced to de-emphasize the idea that inflammation is the cause of pain. Recent studies have shown that patients with diagnosed plantar fasciitis have more disorganization of fibrous tissue, showing degenerative change rather than inflammation. (Schwartz et al, 2014)
Many clients’ main complaint is pain at the heel region – could this be Plantar Fasciitis?
Pain associated with Plantar Fasciitis is usually located on the sole of the heel, or travelling along the sole of the foot, especially the central or inner (medial) aspect of the arch of the foot. Schwartz et al. found that classically, there is severe pain in the morning or after a rest period that improves with movement but is aggravated by long periods of weight bearing, such as walks, runs, or long durations of standing. For example, clients may complain of pain in the morning that improves as they begin moving and walking but is easily flared up from too much activity.
There can be many reasons for heel pain that brings clients in to see their physio, so it is important that they are assessed thoroughly to ensure it is the Plantar Fascia affected. Nerve injuries such as neuropathy are common in diabetics, stress fractures of the heel bone are a common diagnosis in avid runners, and adolescents can suffer from Sever’s Disease (Calcaneal Apophysitis), to name a few.
Physical examination findings are typically tenderness to palpate over the inner aspect of the bone of the heel, and discomfort on stretching of the big toe in an upwards direction.
Why do I have Plantar Fasciitis?
Most clients who suffer from Plantar Fasciitis have taken up a new activity that includes walking or running. Some have increased their loading and training intensity within disciplines they have already been training in. Others have changed the surface on which they are running or walking, such as going from grass to tarmac footpaths or their sports field ground hardening over the summer compared to wetter Winter months. Generally, Plantar Fasciitis occurs when your foot undergoes an increase in load in a short time frame, rather than a gradual change. Sometimes an unsupportive shoe or weak intrinsic foot muscles can contribute to the issue, and time should be given to assess these factors too.
Can I recover from Plantar Fasciitis?
Yes, you can, but how it should be treated may take some deeper thought. Research has been rather vague for treatment of Plantar Fasciitis. Many treatment modalities have been tried and tested, and some have had favorable results, however the quality of these studies is somewhat questionable. Treatment is largely nonoperative, with 90%–95% of patients experiencing resolution of symptoms within 12–18 months with conservative management, according to Dr. Lim and colleagues. In all the literature reviewed, plantar fascia-specific stretching had the best statistically significant long-term results. Using a towel to stretch the toes upwards, and stretching or mobility of the sole of the foot and the calf muscles is most beneficial. Rolling of the sole of the foot with a tennis or hockey ball, or a hard cylinder like a rolling pin or aerosol can is also known to relieve symptoms.
Your physiotherapist can use techniques to help relieve your symptoms. These may include:
- Soft tissue release along the fascia and muscles of the sole of the foot.
- Release of the calf muscles by use of soft tissue management, trigger point therapy, dry needling etc., and passive stretching of the tight structures.
- Implementing a program for strengthening the muscles of the foot and lower leg, to help absorb impact from the ground when running and walking.
- Educating the client on a gradual return to training and how to reach their goals without painful flare ups.
How can we prevent Plantar Fasciitis from developing?
- Slowly increase load: If you are planning on taking up running, walking or a new sport, always take a gradual approach to your training, especially if you are starting from being quite sedentary or inactive. Be patient with your progress, for too quick an increase in load can cause not only Plantar Fasciitis, but other injuries, such as tendinopathies and muscle strains. (see muscle strain blog here)
- Footwear: If you already enjoy a particular exercise, you should ensure you are doing so with the correct footwear. Regardless of your foot-type, your shoes or boots should have enough cushioning and support around the heel and arch of the foot to prevent too much impact being forced upon the Plantar Fascia.
- Listen to your body: If you start developing pain from a certain activity, or notice pain routinely when you wake up in the morning, then see your physio. Tending to these types of injury in the early stages is much more suitable than waiting for symptoms to develop further.
- Strength: Whether it is supervised by a physio or a personal trainer, or you are happy to work alone, a strength program is a great way to prevent these injuries from occurring. Muscle groups that require attention for this particular injury would include the glutes, hamstrings, calves, and intrinsic foot muscles. Taking part in a non-impact cardio exercise, such as cycling, can be very useful to give the Plantar Fascia a break, allowing you to continue working on your fitness.
References:
Kumka M, Bonar J. Fascia: a morphological description and classification system based on a literature review. J Can Chiropr Assoc. 2012;56(3):179-191.
Schwartz EN, Su J. Plantar fasciitis: a concise review. Perm J. 2014;18(1):e105-e107. doi:10.7812/TPP/13-113
Lim AT, How CH, Tan B. Management of plantar fasciitis in the outpatient setting. Singapore Med J. 2016;57(4):168-171. doi:10.11622/smedj.2016069