Meniscus Tears & Physiotherapy
Meniscal Tear Injuries
Can it be managed non-operatively?
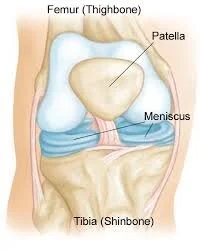
The meniscus is a C-shaped ring of cartilage, found within the knee joint. Each knee has 2 menisci, so therefore we can name them by their position – medial (inner) and lateral (outer) meniscus. The meniscus was once believed to be pretty redundant, and up until the 1970’s, any sort of meniscal tear would be managed with a complete removal of the cartilage ring. Nowadays, we try to protect the menisci as much as possible, and only remove what is totally necessary, if surgical intervention is indicated. Also, physiotherapists have sprung to the forefront of meniscal rehab in recent years, as conservative management of certain meniscal tears has been found to be super effective, rather than just seeking an orthopaedic opinion straight away.
Why is the meniscus so important?
Within the knee, structures called ligaments work to stabilise the joint, for example the ACL prevents too much sliding forward of the tibia, or shin bone. The MCL stabilises the inner aspect of the knee and stops it from buckling inwards. But in addition, the menisci also have stabilising properties. The medial meniscus is a secondary stabiliser to the ACL, and the shape of the menisci helps prevent extreme flexion or extension of the knee. Therefore, it is not uncommon to see meniscal injuries in conjunction with damage to structures such as ACL, PCL, or other bony injuries. It also works as a shock-absorber and helps to keep the hinge joint of the knee moving and gliding smoothly.
Diagnosis of Meniscal Tears
Getting a detailed history from the patient will give physiotherapists a big hint as to what could be the cause of their knee pain. Patients often complain of pain or swelling along the inner or outer border of the front of the knee joint, and report pain during sleeping or lying on their side, due to this tenderness. What helps clinicians to diagnose meniscal injuries as opposed to ligament or joint sprains, is the addition of symptoms such as clicking, locking, grinding, or a sensation of the knee “giving way”. Of course, these symptoms can be present in ligamentous injuries, such as an ACL tear causing lack of stability and the joint “giving way”, but audible clicks and a locking of the knee in either flexion or extension usually indicate a meniscal issue.
Special tests used by physiotherapists help rule in or rule our meniscal issues include Appley’s Grind test and McMurray’s test, but despite these being used for many years, no research has truly proved that they have a high accuracy or reliability (Smith et al., 2015). MRI remains the gold standard for assessing structures within the knee and helps healthcare professionals to identify what aspect of the meniscus is damaged.
Types of Meniscal Tear
Of course, there are many ways a tear can present within the meniscus. See the diagram below for the most common types of tears. These injuries can happen from complex high impact sports injuries such as basketball, skiing, rugby and gymnastics, but can also occur in low impact twists or buckling of the knee in everyday movements.
The location of the tear will be a deciding factor on whether it should be managed surgically or conservatively. This is because different areas of the meniscus have varying blood supplies, therefore the healing in some portions of the cartilage can be poor no matter how much care you take.
Conservative management – what should I expect?
Many meniscus tears can be managed without surgery, especially those without mechanical symptoms such as locking or painful clicking. This rehab period should include relative rest and physiotherapy. You may take oral anti-inflammatories prescribed by your doctor or some patients will undergo corticosteroid injections to manage inflammation if clinically indicated by your specialist.
Early stage meniscal management exercises are used to gently regain motion within the knee joint, strengthen the muscles that support and surround the knee, and to encourage healing and strengthening of the torn tissues.
Remember, many meniscal injuries are in an area called the posterior horn, at the back of the knee. This area is easily irritated by excessively bending, so take care especially when doing standing exercises like squats and lunges. Also, monitor your pain levels. They shouldn’t increase too far past your threshold for pain during exercises, and certainly should subside within 24hrs of your workout. If your pain increases drastically with exercise and lingers afterwards, you are likely pushing a bit too hard.
Exercises in the early stage should focus on:
Cycling. This has been found to be the most suitable conservative exercise for the meniscus as it targets range of motion and strength. It is also great to include as a cardio exercise that doesn’t involve impact on the injured knee, such as in walking or running. Cycling can be done for up to 30 minutes 3-4 times a week, again, once pain is monitored.
Quads muscle strengthening.
Knee range of motion, for example, lying flat and sliding your heel along the ground to straighten and bend your knee.
Increasing weight bearing tolerance and eliminating limp or gait abnormalities.
Balance exercises, beginning with static and then moving to dynamic challenges.
Once your knee starts to tolerate the exercises, and your pain begins to improve, you can increase the difficulty of the exercises, by providing resistance against the quads and hamstring muscles. Squats, and hip hinge exercises can be added, as exercises done in standing can help you progress towards more functional goals and increase joint awareness (proprioception).
After a few weeks, sports-specific drills can be incorporated to assist you returning to changing direction, pivoting, accelerating, and decelerating.
You should consult a physiotherapist to guide you along this pathway and ensure that your program is specific to you. They should be able to help create and reach your goals, and get you back to enjoying your sports, activities, and daily tasks.
Written by Angela Crowley
M.R.S Physiotherapists
References:
Smith BE, Thacker D, Crewesmith A, Hall M. Evid Based Med. 2015 Jun; 20(3):88-97.